THE VBP Blog
Driving Better Outcomes – How Value-Based Payments Advance Florida’s Medicaid Managed Care Program
Florida’s Medicaid Program Strengthens Accountability and Quality Through Value-Based Care

April 10, 2025 – Florida’s Statewide Medicaid Managed Care (SMMC) 3.0 marks a shift in the state’s approach to Medicaid. It introduces a more coordinated and patient-centered model of care. While the program brings many important updates—including expanded benefits, stronger care coordination, and pilot programs for the IDD community—one of the biggest changes lies in its approach to value-based payments (VBP).
SMMC 3.0’s VBP framework requires health plans to integrate performance-based incentives, track provider success, and meet minimum value-based payment thresholds. This blog, the last in our SMMC 3.0 recap, explores the innovative value-based purchasing strategies at the heart of Florida’s Medicaid managed care program.
SMMC 3.0 and VBP – The Basics
A key component of the new Medicaid managed care program in Florida, is the adoption and integration of value-based payments (VBP), which changes how healthcare providers and Managed Care Organizations (MCOs) are reimbursed.
Traditionally, Medicaid has operated under a fee-for-service model. Under this model, providers are paid for the number of services they deliver rather than the quality of care provided. However, this approach often leads to fragmented care, unnecessary procedures, and higher healthcare costs. In contrast, VBP ties provider payments to patient health outcomes, incentivizing high-quality, coordinated care. By rewarding providers for improving patient health outcomes rather than just increasing service volume, Florida is trying to create a more patient-focused Medicaid system.
Key VBP Requirements in SMMC 3.0 – VBP Programs & Transparency
Under SMMC 3.0, value-based payment models are no longer optional. Managed care plans that fall under the Managed Medical Assistance (MMA) Program are required to enter into contracts with providers that link payment to performance. MMA provides Medicaid covered medical services like doctor visits, hospital care, and behavioral health care. Within the MMA program the managed care plan is required to utilize VBP agreements with the providers within its provider network.
Not only are MCOs in Florida’s SMMC 3.0 program required to implement VBP models, but value-based payment integration was something seen throughout the entire ITN (AHCA ITN 010-22/23) that Florida put out when soliciting MCOs to administer the program. The ITN required MCOs to provide information on how many VBP contracts they had in place, number of providers in the network who had a VBP agreement in place, etc. In addition to this, new VBP contractual requirements were included in the ITN as a core provision. MCOs were required to “develop and implement a value-based purchasing (VBP) program to maximize high value care, reduce inappropriate care, and reward best-performing providers,” according to the ITN.
To encourage participation, Florida has established performance-based incentives that reward providers who meet quality benchmarks. These incentives focus on areas like reducing avoidable hospitalizations, improving medication adherence, and enhancing care coordination. Providers who excel in these areas receive enhanced reimbursement, while those who fail to meet minimum standards may face financial penalties. Providers are also required to participate in the Florida Health Information Exchange (HIE) Encounter Notification Service (ENS). The ENS allows providers to securely track and facilitate patient care management that may assist with reducing duplicative treatments.
To maintain transparency and accountability, a health plan’s value-based payments program must include certain elements to ensure transparency to providers so that they understand the reimbursement that they receive. All VBP agreements with providers in their network must include:
- A detailed methodology on how enrollees are assigned to providers for calculation of final payment.
- A detailed methodology on how each provider’s target budget is calculated.
- A detailed methodology on how data will be shared, at least quarterly, between the plan and the provider.
- A detailed list of quality measures used for calculating shared savings or losses.
Transparency is essential to the success of value-based payment models under SMMC 3.0 because it ensures providers understand how they’re being paid and evaluated. Without this clarity, providers may be hesitant to enter into VBP agreements—or worse, deliver care without a clear understanding of how to improve outcomes and meet goals. Ultimately, transparency strengthens the foundation of VBP and increases the likelihood that it will lead to better health outcomes and more efficient use of Medicaid dollars.
Increasing VBP Risk Requirements in SMMC 3.0
What’s unique about SMMC 3.0 is that there is an increasing level of risk taken on by providers and the health plan over the life of the contract. MCOs must use the Learning Action Network (LAN)’s alternative payment framework, which is a nationally recognized system used to classify VBP arrangements based on the level of financial risk and accountability shared between payers and providers.
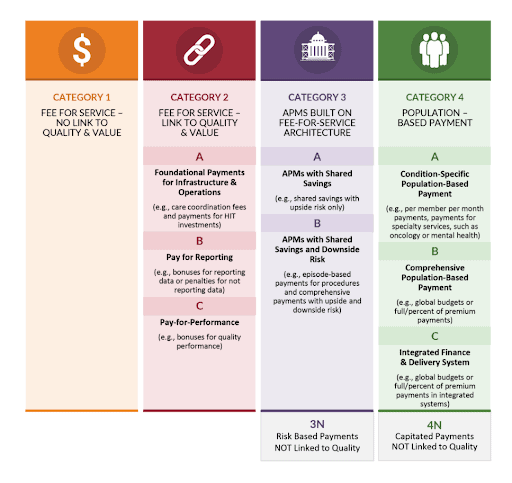
As seen in the chart above, the LAN framework includes four main categories, and within each category are sub-levels that indicate increasing levels of financial risk and sophistication. Florida uses this framework in SMMC 3.0 to set progressive benchmarks for managed care plans, requiring them to move more payments into higher LAN categories over time.
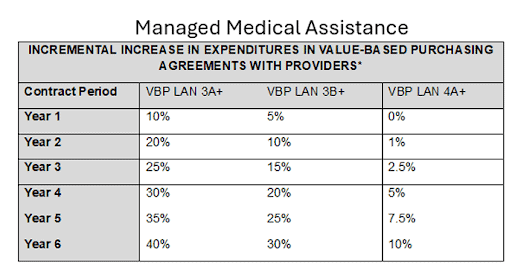
This structure can be seen in the chart above and lends itself to the enhanced level of integration that SMMC 3.0 prioritizes. As the level of financial risk shared by providers and health plans increase through VBP arrangements, it creates a strong incentive to enhance integration across medical, behavioral, and long-term care services. When plans and providers are held accountable for outcomes and costs, coordinated care becomes essential to improving efficiency, avoiding duplication, and delivering better results for enrollees.
Why Do Value-Based Payments Matter in Medicaid Programs?
In contrast to the traditional fee-for-service model, where providers are paid based on service volume, VBP encourages providers to:
- Focus on preventive care to avoid costly hospitalizations and complications.
- Coordinate services across specialties to ensure better patient outcomes.
- Improve efficiency by reducing redundant or unnecessary treatments.
- Address social determinants of health, such as housing and food security, which impact overall well-being.
So, why does are value-based payments so important, especially for Medicaid programs like the one in Florida? Medicaid serves low-income and high-need populations, many of whom face complex medical conditions, disabilities, or social barriers to care. Under a fee-for-service model, providers may not have the financial incentive to invest in preventive services, chronic disease management, or community-based interventions that improve long-term health.
However, under VBP, providers and managed care plans are rewarded for improving patient outcomes, which can lead to lower costs and better health equity. SMMC 3.0 fully embraces VBP as a core principle, requiring Medicaid Managed Care Organizations (MCOs) to implement payment models that align provider incentives with patient health improvements. If done correctly, this shift could create a Medicaid system that prioritizes quality over quantity, and helps ensure that enrollees receive comprehensive, coordinated, and patient-centered care.
Advocate’s Perspective
From an advocate’s standpoint, this shift towards value-based payments in Florida is promising. However, we know it will require sustained attention and oversight. Success depends on more than just policy language. It also hinges on implementation, accountability, and stakeholder engagement. Consumers, especially those with complex needs, must remain at the center of these reforms, and providers must be supported as they navigate this transition. If Florida is successful, its approach to value-based purchasing could serve as a model for other states looking to modernize their Medicaid programs. By linking payment to performance across the entire Medicaid delivery system, SMMC 3.0 offers a roadmap for how to align incentives, improve outcomes, and build a more equitable healthcare system for the future.
Onward!
The newests offering from XtraGlobex:
Dual-Eligible Headquarters
Dual-eligible programs serve a critical role in the healthcare system, providing integrated care for individuals who qualify for both Medicare and Medicaid. CMS plans to align dual-eligible options by 2030, and we are committed to helping you stay ahead of the changes.
The CarePayments Podcast
A quick-hitting informative discussion about healthcare payment models and how they affect MCOs, Providers, Payers, and Care Recipients with your host Fady Sahhar of XtraGlobex.
Listen to The CarePayments Pod
Share This Blog!
Get even more insights on Linkedin & Twitter

About the Author
Fady Sahhar brings over 30 years of senior management experience working with major multinational companies including Sara Lee, Mobil Oil, Tenneco Packaging, Pactiv, Progressive Insurance, Transitions Optical, PPG Industries and Essilor (France).
His corporate responsibilities included new product development, strategic planning, marketing management, and global sales. He has developed a number of global communications networks, launched products in over 45 countries, and managed a number of branded patented products.

About the Co-Author
Mandy Sahhar provides experience in digital marketing, event management, and business development. Her background has allowed her to get in on the ground floor of marketing efforts including website design, content marketing, and trade show planning. Through her modern approach, she focuses on bringing businesses into the new digital age of marketing through unique approaches and focused content creation. With a passion for communications, she can bring a fresh perspective to an ever-changing industry. Mandy has an MBA with a marketing concentration from Canisius College.
