How Florida is Aiming to Make Managed Care Work for Individuals with IDD
Florida is pioneering a managed care pilot for the IDD population with Florida Community Care at the helm
THE VBP Blog

August 8, 2024 – Florida is making strides in improving healthcare services for individuals with intellectual and developmental disabilities (IDD) through a Medicaid managed care pilot program. This initiative, dubbed the Intellectual and Developmental Disabilities (IDD) Pilot Program, is designed to boost the quality of care and coordination for one of the most vulnerable populations.
The IDD Pilot Program will address the complex healthcare needs of individuals with IDD by offering a coordinated approach that includes medical, behavioral, and long-term care services. Florida Community Care, LLC (FCC) has been awarded the contract to manage the program and is tasked with providing comprehensive managed care services that meet the unique needs of individuals with IDD. The award to a single MCO puts into question the ability to separate the program design from the execution of the single MCO. The advocates have expressed concerns about the lack of consumer choice built into the award. The history of FCC also presents challenges that may be more evident in the execution.
In this blog, we will explore the details of this pilot program, its potential impact on individuals with IDD, and how this can be used as a roadmap for future broader implementation of managed care for individuals with IDD.
Florida’s Comprehensive IDD Medicaid Managed Care Pilot to Launch in 2024
In November 2023, the Florida Agency for Health Care Administration (AHCA) took a step towards potentially improving care for individuals with IDD by releasing an invitation to negotiate for a pilot to move support services for people with IDD to managed care.
The pilot will move 600 beneficiaries with IDD to managed care, where they will receive an integrated medical, long-term care, and home-and-community based services (HCBS) waiver services. These individuals currently receive HCBS on a fee-for-service (FFS) basis through the Developmental Disabilities Individual Budgeting waiver (iBudget). This pilot will enroll those 18 years and older with IDD who are eligible for iBUdget services into the Intellectual and Developmental Disabilities (IDD) Pilot Program, also known as the Developmental Disabilities Managed Care Pilot Program.
According to the ITN, the goals of the pilot program are to:
- Maximize managed care flexibility to provide additional services.
- Increase access to HCBS provider organizations and services.
- Maintain highest quality of care coordination and person-centered care plans.
- Increasing opportunities for community integration.
A key advantage of this approach is the flexibility afforded the MCO to add and move services without significant administrative burdens. Responses to the ITN were scored on five criteria, including ability to provide person-centered care, ability to increase access to providers and services, and ability to provide services integrated with the community, among others. Florida Community Care and Simply Healthcare were the sole respondents by the December 8, 2023, deadline.
Florida Awards Florida Community Care to Pilot Comprehensive IDD Managed Care
Florida ACHA reviewed both ITN responses and awarded FCC 983 points out of 1,000, and Simply Healthcare 938 points out of 1,000. Based on this, ACHA awarded a six-year contract to Florida Community Care, LLC, to pilot a managed care program specifically for individuals with intellectual and developmental disabilities (IDD). The pilot program, set to launch in 2024 and run for six years through September 2030 in Medicaid regions D and I.
Historically, individuals with IDD receiving waiver services have been excluded from Medicaid managed care enrollment. The new pilot program marks a shift in policy, as the state tries to create a more streamlined and efficient care model that ensures better health outcomes and coordinated services for this vulnerable population.
Under the old FFS model, services were provided and billed based on the quantity provided, with no particular emphasis on quality. This could mean lack of coordinated care, less personalized care plans, and even duplicate and unnecessary services provided. The new pilot program creates a value-based payment model that will reward providers based on the quality of care provided and health outcomes. The timing of the implementation of the VBP programs could distract the MCO and the providers from the primary purpose of improving the quality of care and supports.
The new pilot program has ambitious goals, the first of which is an emphasis on person-centered care that tailors care plans to the specific needs and preferences of an individual. Florida Community Care will be responsible for collaborating with consumers, families, and a network of providers to ensure comprehensive support across all areas of life. These services include a variety of social, medical, behavioral, therapeutic, and residential services like personal supports, day activities, supported living, therapies, and other long term care waiver services. This is a big ask, as FCC will be tasked with maintaining the high quality standards that the IDD population deserves, while also managing the vast network of providers required to provide the required services and supports.
Making Managed Care Work for the IDD Population
Now that the contract for the Intellectual and Developmental Disabilities Managed Care program is awarded and set to launch this year, it’s important to consider what this can mean for consumers and how we can use this as a roadmap for statewide implementation and beyond.
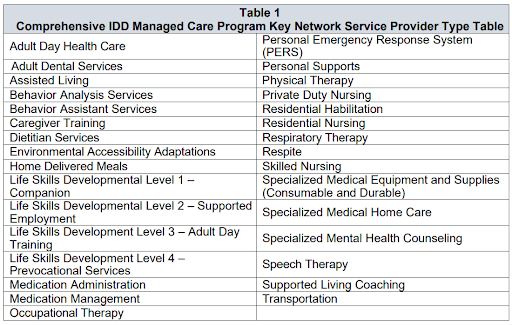
Perhaps the biggest benefit for beneficiaries with IDD in moving over to the pilot program is access to expanded services. The table below from the ITN shows the wide variety of services that will be provided through the pilot program. Not only will the services provided—and covered—be expanded, but so will access to the services. Many individuals needing these services are put on a wait list, but the VBP model
It is also important to note that successfully transitioning individuals with IDD to managed care requires a strategic approach that addresses their unique needs. That is where personalized care plans come into the mix. For successful implementation of managed care for individuals with IDD, these plans should be comprehensive, incorporating medical, behavioral, and social needs. MCOs, like Florida Community Care and any future plans, must ensure collaboration between individuals, their families, and care providers to develop these tailored care plans and ensure continuity of care. This process not only involves a detailed assessment of the individual’s health status, personal goals, and environmental factors to create a plan, but also regular reassessments are crucial to ensure that the care plans remain relevant and responsive to any changes in the individual’s condition or circumstances.
Another essential aspect for making managed care work for the IDD population is the integration of services to ensure that individuals receive whole-person and coordinated care. This involves combining primary care, specialty care, and HCBS to reduce fragmentation of care. Care coordination is also a cornerstone of successful IDD managed care. Care coordinators act as essential liaisons between the individual, their family, and various healthcare providers, ensuring seamless delivery of services. They play a critical role in monitoring the individual’s progress, addressing any issues that arise, and ensuring that the care plan is followed meticulously. This can prevent gaps in care, which is especially important for this population with complex needs to reduce hospital readmissions and emergency room visits, while allowing them to live as independently as possible.
Something else to consider when implementing managed care for individuals with IDD is how to effectively leverage technology to enhance care delivery. For example, telehealth services can provide convenient access to healthcare professionals without the need for travel, which can be challenging for individuals with IDD. Electronic health records (EHRs) and care management platforms can improve access to care and facilitate better communication among care teams, ensuring that all providers have up-to-date information about the individual’s health status and care needs. To take things a step further, assistive technology like communication devices, mobility aids, and smart home systems, can help individuals perform daily activities, communicate more effectively, and stay safe in their environments. By incorporating these technological solutions into care plans, managed care programs can enhance the autonomy and quality of life for individuals with IDD.
When it comes to making managed care work the individuals with IDD, social determinants of health (SDoH) cannot be overlooked. This is especially important because, as the figure below shows, over half of health outcomes are linked with behavior and the environment and not medical care.
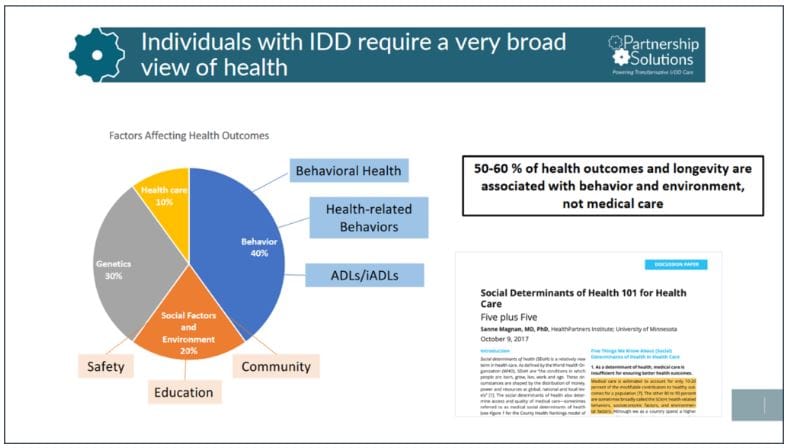
Things like housing stability, transportation, and access to nutritious food significantly impact health outcomes and it is essential that managed care programs include strategies to address these. The good news is that many of these services, like dietician services, transportation, etc. are included in the list of services that must be provided in the IDD pilot program.
Last, but not least, there needs to be continuous monitoring and evaluation of managed care programs to ensure they are meeting the needs of the IDD population. This includes tracking health outcomes, satisfaction levels, and service utilization. This is something that is especially important for the Intellectual and Developmental Disabilities (IDD) Pilot Program because it is a pilot program that can be tested and tweaked to find what works best and improve the program for potential statewide rollout. There are currently 35,000 Floridians enrolled in the iBudget program, with another 22,000 on a waiting list for services. With a lot of back and forth about whether these individuals can be rolled into managed care, this pilot program is set to test that, and must be properly monitored and evaluated to ensure that this vulnerable population with complex needs gets the quality care they deserve.
Advocates Perspective
Florida isn’t alone in its shift to managed care for individuals with IDD. In fact, many other states like North Carolina, Iowa, and more, have committed to the shift. It is important to note that making managed care work for the IDD population in Florida requires a multifaceted approach that prioritizes personalized care plans, integrated services, care coordination, and ongoing provider support. By involving families and caregivers, leveraging technology, addressing social determinants of health, MCOs have the potential to create a supportive and effective care system for individuals with IDD through the IDD pilot program. However, as noted, there needs to be careful monitoring and evaluation to ensure that the needs of this complex population are being met and that there are strides to improve health outcomes and quality of life. The difficulty with this, in that only a single MCO was awarded the contract, could be trying to sort out the program design success or failure, from the success or failure of the single MCO. There is also some lack of consumer choice with the single MCO model, and FCC also a shaky history in the state. As the program progresses, it will be essential to stay informed and engaged, and carefully monitor all aspects of the program. The goal is to ensure success and determine a model for scalability, but only time will tell if Florida finds success with this model.
Onward!
Share This Blog!
Get even more insights on Linkedin & Twitter

About the Author
Fady Sahhar brings over 30 years of senior management experience working with major multinational companies including Sara Lee, Mobil Oil, Tenneco Packaging, Pactiv, Progressive Insurance, Transitions Optical, PPG Industries and Essilor (France).
His corporate responsibilities included new product development, strategic planning, marketing management, and global sales. He has developed a number of global communications networks, launched products in over 45 countries, and managed a number of branded patented products.

About the Co-Author
Mandy Sahhar provides experience in digital marketing, event management, and business development. Her background has allowed her to get in on the ground floor of marketing efforts including website design, content marketing, and trade show planning. Through her modern approach, she focuses on bringing businesses into the new digital age of marketing through unique approaches and focused content creation. With a passion for communications, she can bring a fresh perspective to an ever-changing industry. Mandy has an MBA with a marketing concentration from Canisius College.
