Proposed CMS Rule Would Expand Home Health Value-Based Purchasing Model
Proposed rule would accelerate the shift to a system that pays for value and quality by proposing a nationwide expansion of the Home Health Value-Based Purchasing (HHVBP) Model
THE VBP Blog
On June 28, 2021, the Centers for Medicare & Medicaid Services (CMS) announced a proposed rule that is designed to improve home health care for older adults and those with disabilities. The proposed rule calls for a nationwide expansion of the Home Health Value-Based Purchasing (HHVBP) Model. Under the rule, the HHVBP Model would be expanded to all Medicare-certified Home Health Agencies (HHAs) in all 50 states and the District of Columbia starting January 1, 2022.
Original HHVBP Model
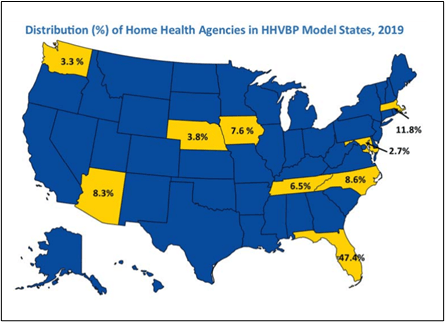
The HHVBP Model was first implemented on January 1, 2016, in 9 randomly selected states that represented each geographic area in the nation: Arizona, Florida, Iowa, Massachusetts, Maryland, Nebraska, North Carolina, Tennessee, and Washington.
The Model was designed to test whether providing payment incentives based on better quality of care with great efficiency would improve the delivery and quality of home health care services for Medicare beneficiaries. The original nine states under the HHVBP Model competed on value, with payments tied to quality performance.
Positive HHVBP Model Results Lead to Proposal for Expansion
After years of reporting and analysis, CMS announced on January 8, 2021, that the HHVBP model met the statutory requirements for expansion. The original HHVBP Model resulted in Performance Scores that were 8% higher among HHAs in HHVBP states than HHAs in non-HHVBP states in 2019. It also reduced cumulative Medicare spending by $604.8 million between 2016 and 2019.
Based on the positive results, CMS is proposing to expand the HHVBP Model nationwide effective January 1, 2022. By expanding the HHVBP Model, CMS seeks to improve the beneficiary experience by providing incentives for HHAs to provide better quality of care with greater efficiency.
“This Model is a great example of how the Innovation Center can design successful models that both improve quality for Medicare beneficiaries and lower costs,” said CMS Innovation Center Director Brad Smith. “Over the past year, we have taken a data-driven approach to assessing all the Innovation Center’s models, and we are excited that HHVBP has met our gold standard for expansion as laid out by Congress.”
HHVBP Model Improved Quality of Care
The HHVBP Model expansion must be implemented through rulemaking, which is what prompted the proposed rule from CMS. While the HHVBP Model resulted in a 1.3% reduction in cumulative Medicare spending, it is important to look at the potential the nationwide expansion has on the quality of care received.
Approximately 70% of those receiving home care in the U.S. are over 65 years of age. Of those individuals, 80% choose to live independently in the comfort of their home, with the majority needing assistance with tasks like bathing and getting in and out of bed. By expanding the HHVBP Model nationwide, those across the country can receive quality and covered services from Home Health Agencies that allow them to remain in their homes. The expansion of the HHVBP not only reduces the chance of individuals having to move to a nursing home or residential care community but also improves their quality of life.
“Homebound Medicare patients face a unique set of challenges and barriers to getting the care they need,” said CMS Administrator Chiquita Brooks-LaSure. “[This] announcement is a reaffirmation of our commitment to these older adults and people with disabilities who are counting on Medicare for the health care they need. This proposed rule would streamline service delivery and value quality over quantity – at a time when Americans need it most.”
Advocate’s Perspective
With HHVBP’s test model tapping at the core of what value-based is about, we think this expansion is ringing all the right bells for VBP. Expanding this program nationwide will keep residents at home, out of nursing facilities, increase the quality of care, and reduce costs. While the model set will see some challenges as it expands, the stats support this as a positive decision for consumers, which is always our main objective.