The Results Are In – Medicare Shared Savings Program ACOs Are Reducing Costs and Improving Care
Shared Savings Program yielded more than $2.1 billion in net savings in 2023, but that’s not all.
THE VBP Blog

November 15, 2024 – The Medicare Shared Savings Program (MSSP or Shared Savings Program) has become a cornerstone of Medicare’s efforts to transition from traditional fee-for-service to value-based care. Recently, the Centers for Medicare & Medicaid Services (CMS) announced the Shared Savings Program results for 2023, revealing significant savings and improved performance.
In this blog, we will explore how the Medicare Shared Savings Program works and analyze the 2023 results. We’ll also look at the program’s benefits for patients, providers, and the broader healthcare system.
What is the Medicare Shared Savings Program?
The Medicare Shared Savings Program is a value-based payment initiative established by CMS in 2012. Its primary goal is to encourage healthcare providers to form Accountable Care Organizations (ACOs) that work to improve the quality of care for Medicare beneficiaries while reducing unnecessary healthcare spending.
In this program, ACOs are made up of groups of doctors, hospitals, and other healthcare providers who voluntarily collaborate to manage and coordinate care for Medicare beneficiaries. These ACOs are incentivized to meet specific quality benchmarks and achieve savings targets. If an ACO successfully reduces costs while maintaining or improving care quality, it shares in the savings with Medicare. This shared savings model encourages providers to focus on preventive care, chronic disease management, and reducing avoidable hospitalizations, all of which contribute to lower healthcare spending and improved patient outcomes.
Source: CMS
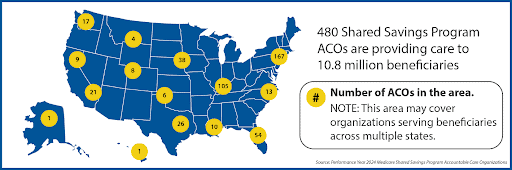
Currently, there are 480 ACOs in the Shared Savings Program, with over 608,000 clinicians providing care for nearly 11 million beneficiaries.
In this program, ACOs are made up of groups of doctors, hospitals, and other healthcare providers who voluntarily collaborate to manage and coordinate care for Medicare beneficiaries. These ACOs are incentivized to meet specific quality benchmarks and achieve savings targets. If an ACO successfully reduces costs while maintaining or improving care quality, it shares in the savings with Medicare. This shared savings model encourages providers to focus on preventive care, chronic disease management, and reducing avoidable hospitalizations, all of which contribute to lower healthcare spending and improved patient outcomes.
Shared Savings Program Modeled for Different Levels of VBP
Under the Shared Savings Program, ACOs are offered two primary participation tracks, the BASIC Track and the ENHANCED Track. These tracks are based on varying levels of experience and readiness to assume financial risk.
The Basic Track is designed to help newer or smaller ACOs gradually transition into a value-based care model with increasing levels of risk and reward. It features a “glide path” consisting of five levels that allow ACOs to start with a one-sided risk model and eventually move to a two-sided risk model. The first two levels operate under a one-sided shared savings arrangement, where ACOs can share in any cost savings they achieve without being liable for financial losses. This provides a low-risk entry point, allowing ACOs to build experience in managing costs and improving care quality without facing financial penalties. As ACOs progress, they transition into a two-sided risk model, where they can share in a larger portion of the savings but also assume responsibility for a percentage of any losses. By the last level, ACOs are fully accountable for both savings and losses.
The Enhanced Track is aimed at more experienced ACOs that are ready to assume full two-sided risk from the start. Under this model, ACOs share a larger portion of both savings and losses, which allows for potentially higher financial rewards but also requires them to be accountable for any cost overruns. This track is designed for ACOs with an established ability to manage patient populations, control spending, and deliver high-quality, coordinated care.
By offering both the Basic and Enhanced Tracks, MSSP enables ACOs to select the level of risk that matches their experience and resources, promoting a pathway toward full accountability and value-based payments. This flexibility and slower progression can incentivize ACOs that are interested in participating, but that need some time to ramp up their infrastructure and experience.
For home health consumers, particularly those managing chronic conditions, VBP emphasizes care coordination, ensuring that all aspects of their care—nursing, physical therapy, medication management—are integrated. This leads to fewer communication gaps between providers and a smoother healthcare experience. It also, according to the most recent HHVBP Model Annual Report, leads to lower hospitalization rates.
Additionally, because VBP models reward providers for keeping patients healthy, consumers are more likely to receive timely care and interventions that help them stay at home longer, preventing costly hospital stays or nursing home placements. According to research, home health providers who operate under VBP models have demonstrated reduced costs for consumers while improving their overall health outcomes.
Ultimately, VBP enhances the home health experience by ensuring that care is both efficient and effective, with a strong focus on patient well-being and long-term health. We are also optimistic about the impact that value-based payment models can have on the home care industry, as that seems to be the next frontier of VBP.
Shared Savings Program Generating Cost Savings and Performance Improvements
The Medicare Shared Savings Program (MSSP) has continued to demonstrate substantial financial savings and improvements in care quality since its launch. According to recent reports from CMS, MSSP ACOs saved Medicare $2.1 billion in 2023, the highest savings recorded in the program’s history, including the $1.8B achieved in 2022. This brings the cumulative savings for Medicare since MSSP’s inception in 2012 to over $21 billion. These savings highlight the program’s effectiveness in driving healthcare providers to manage costs more efficiently without sacrificing patient care quality.
Quality of care is paramount, and the Shared Savings Program delivered here as well. From performance year (PY) 2022 to PY 2023, ACOs showed improvement on quality measures as well. This includes statistically significant improvement on quality measures related to diabetes and blood pressure control, breast cancer and colorectal cancer screening, screening for future fall risk, statin therapy for prevention and treatment of cardiovascular disease, and depression screening and follow-up. Through whole-person and coordinated care, as well as proactive management of chronic diseases and emphasis on preventive services, ACOs help keep patients healthier and reduce the likelihood of expensive interventions
In 2023, over 90% of participating ACOs met or exceeded quality benchmarks. 453 of the 480 ACOs achieved shared savings, and together, shared in the $3.1 billion distributed as shared savings through the program. By incentivizing ACOs to meet or exceed performance measures, the program can demonstrate that it’s possible to enhance care quality and outcomes while still being profitable.
Advocates Perspective
Based on past and recent results, it’s clear that the Medicare Shared Savings Program can improve care quality and reduce costs for Medicare beneficiaries. By focusing on preventive care, chronic disease management, and coordination between providers, the MSSP helps keep patients healthier while reducing unnecessary healthcare costs. If ACOs continue to balance financial goals with patient-centered care, especially for those with complex health needs, the program has great potential. However, we need to be sure to address equity in the MSSP, ensuring that all beneficiaries, including underserved populations and those in rural areas, receive the same level of attention and access to care enhancements. With careful oversight, the MSSP can be a powerful tool for advancing value-based care while safeguarding patient interests.
Are you wondering what is next for the Medicare Shared Savings Program? CMS just released the 2025 Medicare Physician Fee Schedule Final Rule, and it includes several provisions related to the MSSP. Stay tuned for our VBP blog next week where we will explore these provisions and what they mean for consumers!
Onward!
Share This Blog!
Get even more insights on Linkedin & Twitter

About the Author
Fady Sahhar brings over 30 years of senior management experience working with major multinational companies including Sara Lee, Mobil Oil, Tenneco Packaging, Pactiv, Progressive Insurance, Transitions Optical, PPG Industries and Essilor (France).
His corporate responsibilities included new product development, strategic planning, marketing management, and global sales. He has developed a number of global communications networks, launched products in over 45 countries, and managed a number of branded patented products.

About the Co-Author
Mandy Sahhar provides experience in digital marketing, event management, and business development. Her background has allowed her to get in on the ground floor of marketing efforts including website design, content marketing, and trade show planning. Through her modern approach, she focuses on bringing businesses into the new digital age of marketing through unique approaches and focused content creation. With a passion for communications, she can bring a fresh perspective to an ever-changing industry. Mandy has an MBA with a marketing concentration from Canisius College.
