VBP Update – What are Value-Based Payments?
Exploring the Basics and Models of Value-Based Payments
THE VBP Blog

October 10, 2024 – Value-based payments (VBP) are changing the way healthcare providers deliver care, focusing on quality and health outcomes rather than the traditional fee-for-service model. In VBP, providers are rewarded for delivering high-quality care that improves health, while reducing unnecessary costs and inefficiencies. This approach incentivizes preventive care, better management of chronic conditions, and overall well-being.
As value-based payments become more prevalent across the healthcare industry, we are seeing them shift into non-medical applications like home care. This can have a big impact on the lives of seniors, the IDD community, and those managing chronic conditions. As this shift continues, value-based payments are being pushed towards the forefront, which is why it’s important to have a thorough understanding of them. That’s what we’re here to help with by providing a mini VBP Refresher Series, where we’ll discuss things like:
- What value-based payments are
- The history of VBP
- Key value-based payment models
- The VBP Continuum
- Benefits of utilizing value-based payments
- Current VPB programs being used and their results
- The shift towards value-based payments in home care
In this blog, the first of our VBP Update series, we break down the basics of value-based payments, its history, key payment models used, and the value-based payment continuum. Let’s dive in!
History of Value-Based Payments
The shift towards value-based payments (VBP) emerged as a solution to the inefficiencies of the traditional fee-for-service (FFS) model. In a fee-for-service system, providers are paid for each service or procedure provided, regardless of the results or necessity. This often led to consumers being subjected to unnecessary tests and treatments, higher overall healthcare costs, and less personalization of care plans.
The movement toward VBP gained significant momentum with the passing of the Affordable Care Act (ACA) in 2010. The ACA introduced reforms to expand access to care, reduce healthcare costs, and promote value-based care. It established accountable care organizations (ACOs) and introduced the Hospital Value-Based Purchasing Program. This marked a significant shift in how healthcare providers were paid, rewarding those who offered better care rather than simply more care. The CMS Innovation Center was also founded in 2010, and has been instrumental the development and implementation of new payment and service delivery models.
Since then, in addition to Medicare’s reforms, private insurers and Medicaid programs began adopting similar models, leading to broader acceptance of VBP across the healthcare system. Accountable Care Organizations (ACOs), bundled payments, and patient-centered medical homes became popular models under the VBP umbrella.
In 2012, we also started to see a shift towards value-based payments in the non-medical sectors like home health. This is an area that is still undergoing a transformation and something we think can have a major impact on helping individuals with IDD or chronic diseases, and seniors remain safely and live independently in their homes.
What Are Value-Based Payments?
Value-based payments (VBP) are healthcare payment models that reward providers for delivering high-quality care and improving health outcomes, rather than paying based on the number of services provided. The goal of these models is to create a more efficient healthcare system, that uses innovation to improve quality while also managing costs. Below are the main types of value-based payment models that we see in the healthcare industry:
Performance-Based Payment: In performance-based payment models, healthcare providers are rewarded based on the quality of care they deliver, measured against specific performance metrics. These metrics usually focus on processes rather than outcomes. Providers who meet or exceed these targets are financially rewarded. This model encourages a focus on preventive care, early intervention, and ongoing management of health conditions.
Bundled Payment: The bundled payment model provides a single, predetermined payment for all the services linked to a particular condition or procedure, like a surgery or hospital stay. This lump sum covers pre-care, the procedure itself, post-operative care, and rehabilitation. By receiving a set amount, healthcare providers are incentivized to coordinate care efficiently and reduce unnecessary costs. This model encourages collaboration among providers, as they work together to manage the care within the budget while maintaining or improving quality standards.
Shared Savings and Risk: Shared savings and risk models incentivize healthcare providers to lower overall healthcare costs while maintaining or improving quality. Under shared savings models, providers are rewarded for reducing healthcare costs while maintaining or improving quality. If care is delivered more efficiently than expected, providers share in the financial savings. Under shared risk, providers take on more responsibility by sharing in both savings and potential losses. If costs exceed the agreed-upon budget, providers are held accountable and must cover part of the financial losses, encouraging greater efficiency and accountability. This approach promotes efficient, coordinated care and encourages providers to take responsibility for managing resources effectively. It is commonly used in models like ACOs, where a group of providers work together to manage the health of a specific patient population.
Capitation: Capitation is a payment model in which healthcare providers receive a fixed amount per consumer for a specified period, regardless of the number or type of services provided. Providers are incentivized to focus on preventive care and managing patient health effectively to avoid costly interventions. Capitation encourages efficiency by placing the financial risk on providers to deliver necessary care within a set budget. This model is often used in primary care settings, where the focus is on keeping patients healthy through regular check-ups, screenings, and early interventions.
As you can see, there are many different type of value-based payment models, and each has its own risks and rewards associated with it. This is what we call the VBP continuum.
What is the Value-Based Payment Continuum?
The continuum of value-based payment (VBP) models represents a progression in how providers are reimbursed, shifting from volume-driven to value-driven care. Below is a chart that shows the progression of VBP models based on the level of risk taken on by the provider.
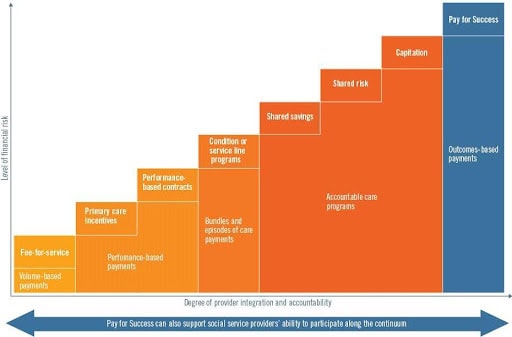
Once we move beyond FFS, at the simplest level is performance-based payment. This is where providers are financially rewarded for meeting specific quality metrics, without assuming major financial risks. The next step is bundled payments, where a single payment is provided for all services during a specific episode of care. As we move along the continuum, shared savings and risk models allow providers to share in financial gains if they reduce healthcare costs while maintaining quality, but also assume responsibility for losses if they exceed cost targets. Capitation, at the far end of the spectrum, gives providers a fixed, per-patient payment that covers all necessary care, regardless of how much or how little care the patient requires. Providers under capitation must manage the patient’s overall health while containing costs, as they bear full financial risk.
This continuum reflects the increasing level of risk and responsibility that providers must take on as they move from basic performance-based models to full capitation. Each model on the continuum aims to align financial incentives with the goal of delivering better health outcomes, gradually transitioning providers to assume greater financial accountability for the care they deliver.
Advocates Perspective - Is There a Better Option?
Value-based payment (VBP) models offer promising advancements in healthcare, and under certain models we have already seen improved patient outcomes, reduced hospital readmissions, and cost-reductions. These models shift the focus from volume to value, ensuring that consumers receive higher quality, coordinated care. As VBP has shown promise in medical settings, we are now seeing it transition into non-medical hone care field. This is something that has great promise and we are excited to see how it can be implemented to allow individuals to remain living independently at home. However, as we transition to VPB models, there is still the challenge of ensuring equitable access, especially for vulnerable populations with complex health conditions. To fully realize the potential of VBP, it’s crucial to strike a balance between efficiency and fairness. That is why continuous monitoring and tweaks needed to ensure VBP works for all consumers.
Stay tuned for our next blog in the VBP Update Series! Next week we will dive into the benefits of value-based payment models for consumers, providers, and payers.
Onward!
Share This Blog!
Get even more insights on Linkedin & Twitter

About the Author
Fady Sahhar brings over 30 years of senior management experience working with major multinational companies including Sara Lee, Mobil Oil, Tenneco Packaging, Pactiv, Progressive Insurance, Transitions Optical, PPG Industries and Essilor (France).
His corporate responsibilities included new product development, strategic planning, marketing management, and global sales. He has developed a number of global communications networks, launched products in over 45 countries, and managed a number of branded patented products.

About the Co-Author
Mandy Sahhar provides experience in digital marketing, event management, and business development. Her background has allowed her to get in on the ground floor of marketing efforts including website design, content marketing, and trade show planning. Through her modern approach, she focuses on bringing businesses into the new digital age of marketing through unique approaches and focused content creation. With a passion for communications, she can bring a fresh perspective to an ever-changing industry. Mandy has an MBA with a marketing concentration from Canisius College.
