What is Value-Based Payment?
- A desire for payment reform and better coordination sparked the Value-Based Payment model
- The adoption of value-based care is expected to account for 59% of all healthcare payments by 2020
- Realizing success in a VBP model requires innovative business models & skill in population health management
Value-Based Payments: The Basics
The United States spends twice as much on healthcare as other wealthy countries—$10,384 vs. $5,169 on average, respectively—but sees significantly worse health outcomes than those same countries. Value-based care programs are a way to close that disparity.
Under value-based payment (VBP) models, payments to healthcare providers are tied to quality, efficiency, and positive patient experience. The purpose of value-based programs is to improve care for individuals and lower healthcare costs simultaneously.
With this delivery model, doctors, hospitals, and other health care providers are compensated based on the quality of care provided and patient outcomes. In the traditional Fee-For-Service (FFS) model, healthcare providers are paid for the quantity of services provided, and compensation has nothing to do with the results of those services. Under a value-based care model, providers are rewarded financially for providing high quality, cost-effective care.

The Benefits of Value-Based Care
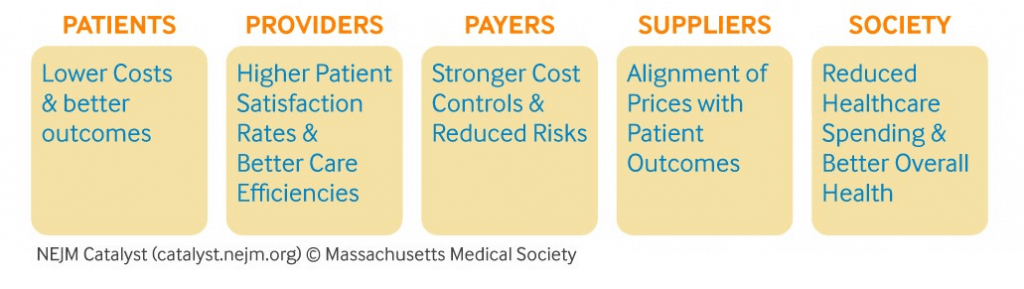


Patients
Providers
Patients spend less money and receive better care because these models are designed to encourage providers to help patients recover from injuries and illnesses more quickly. This means fewer visits to the doctor, fewer medical tests and procedures, and less prescription medication costs. For patients with chronic conditions like cancer, high blood pressure, or obesity, value-based payment models allow them to receive better care at a lower cost.
Providers also benefit from value-based care because they establish greater efficiencies and patient satisfaction. More time may be spent up front developing prevention-based services, but ultimately, providers will spend less time managing chronic diseases and conditions. In addition, their patient satisfaction rates will rise when the focus is placed on the quality of care instead of the volume of services provided.

Payers
Suppliers
Payers also reap the benefits of a value-based payment model by reducing risk and costs. By spreading care across a larger patient base, the risk is reduced. A healthier population with fewer insurance claims means fewer expenses pulled from the premium pools and more money going to the bottom line. In addition, payers can also bundle payments to cover the full cycle of care for a patient, which allows for increased efficiency and further reduced costs.
In a value-based care system, suppliers are also encouraged to align prices with outcomes. They will benefit from aligning services and products, like prescription drugs, with positive patient outcomes and reduced expenses. This becomes easier for suppliers with the growth of individualized therapies encouraged in a value-based payment model.
Need more help understanding Value-Based Payments? Contact XtraGlobex Today!
Common Value-Based Payment Models

Under the umbrella of value-based care, there is a variety of different value-based payment models. These models come with varying degrees of provider accountability and generally differ as to the risks assumed by providers and the sharing of savings or losses.
Value-based care is still a new concept for most healthcare providers and many are still trying to implement the appropriate systems into their workflow.
Pay for Performance
Bundled Payments
Capitation
Accountable Care Organization
In a Pay for Performance system, payers compensate providers for meeting specific pre-established measures for efficiency and quality. PFP programs are utilized by both private insurers and Medicare, but this model is often used primarily as an overlay for FFS payments because bonuses have proved insufficient to encourage the necessary changes.
Bundled Payments are single payments for a group of services that are related to a specific condition or treatment that may involve multiple providers across different settings. A predetermined fee is established to provide all services associated with a given procedure to encourage providers to offer quality and cost-effective care.
The Capitation model sees providers taking full financial responsibility for a specific patient population. Members pay a fixed annual premium, which is then pooled together to fund the care of the entire population segment. Through this model, providers are encouraged to spend funds in a way that will maximize the health of the total population.
ACOs are groups of physicians, doctors, hospitals, and other health care providers that come together voluntarily to provide high-quality, coordinated care to Medicare patients. The goal of an ACO is to ensure that chronically ill patients get coordinated care at the right time and avoids unnecessary duplication of services.
Shared Savings
Shared Risk
Medicare Quality Incentive Programs
Payment for Coordination
Under a Shared Saving model, payers set a budget for care-delivery costs. Providers with total costs below that budget then share in the overall savings. This is not a value based payment model in itself but is often used in conjunction with other VBP models to encourage quality care at reduced costs.
Another option for a value based care model is Shared Risk. This is similar to shared savings in that providers will still share the overall savings, but under this model, they are also expected to pay for care delivery costs that exceed the cost of care budget set by the payer.
Medicare Quality Incentive Program is a pay-for-reporting program. Although PQRS is a standalone program, it touches on other CMS programs that require quality reporting. This program provides incentives to eligible professionals and payment adjustments for correctly reporting quality measures.
Payment for Coordination involves payment for specified care coordination services. In a medical or health care home scenario, the medical home is given a monthly payment in exchange for coordinating care services that would not otherwise be provided or reimbursed.
Why Value-Based Care Models Matter

In 2017, U.S. healthcare spending reached a staggering $3.5 trillion and accounted for 17.9 percent of the nation’s Gross Domestic Product (GDP). Spread out across the population, that’s $10,739 per person.
Under the current Fee-For-Service (FFS) model, physicians and healthcare providers deliver services and the cost for their services has little to do with the outcome. This led to an increase in out of pocket healthcare expenses.
In just one year, out of pocket expenses in the U.S. rose from 1.9% to 4.3%. This rise in health care costs is due to a lack of coordination between providers and limited preventative actions. With costs expected to rise even higher, a desire for a better payment model emerged.
Under the value-based payments model, healthcare providers are paid in accordance with the quality, not the quantity of their care. While VBPs only accounted for 25% of healthcare payments in 2015, in 2017 that number reached 34%. It is expected to continue rising. In fact, by 2020, value-based care is expected to account for 59% of all healthcare payments. Some insurance providers are placing even higher importance on value-based care. Aetna, for example, is striving for 75% to 80% of payments through value-based care models by 2020.
Moving from an FFS to a VBP system takes time, but like it or not, value-based payment models are only going to increase in importance in the coming years as the healthcare industry continues to evolve. That is why it’s important to get on board now. Value-based care is being embraced as the best method to increase the quality of care while lowering healthcare costs, and more and more providers are adopting these payment models. If you are looking for assistance with value-based payments, contact XtraGlobex!
Get the blog for free right to your inbox
Not ready to start the project but want insider access to our expert insights? Subscribe now to trending topics and tips direct to your inbox.